Social Welfare
Affordable and Accessible Healthcare for All
Posted On:
17 JUN 2025 9:33AM
Introduction
From 2014 to 2025, India’s healthcare system has undergone a profound transformation under the dynamic leadership of Prime Minister Narendra Modi. With a people-first approach, the government has focused on making quality healthcare accessible and affordable to all citizens, especially the underprivileged and rural populations. Whether it’s the world’s largest health insurance scheme, Ayushman Bharat, or the far-reaching eSanjeevani telemedicine platform, the focus has been clear: affordable, accessible, and accountable healthcare for all.
India didn’t just navigate the COVID-19 crisis—it led from the front, administering over 220 crore vaccine doses and emerging as a global health partner to the world. Preventive care has surged through mass immunisation campaigns like Mission Indradhanush. Medical education has been overhauled, with a record expansion of AIIMS institutions and MBBS seats, empowering a new generation of doctors from every corner of the country. Generic medicines have become easily available through Jan Aushadhi Kendras, saving families lakhs in medical expenses.
This is not just a story of infrastructure—it is a story of impact. Maternal deaths are down. Access is up. Confidence in the public health system has never been stronger. As India enters Amrit Kaal, its health journey is no longer just about treating illness—it’s about nurturing a nation. Health has become a right, not a privilege. And under the Modi Government, every Indian life matters—with dignity, care, and hope at the core.
Universal Health Coverage through Ayushman Bharat
- Ayushman Bharat- Pradhan Mantri Jan Arogya Yojana (PM-JAY)
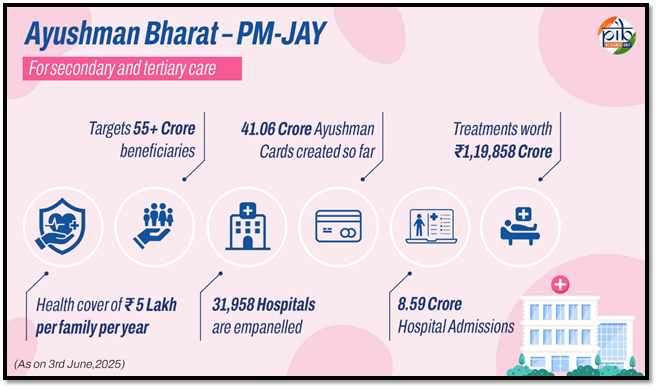
In 2018, the government launched Ayushman Bharat- Pradhan Mantri Jan Arogya Yojana (PM-JAY), the world’s largest health assurance programme, with an aim at protecting economically vulnerable Indians from catastrophic healthcare expenditures. Targeting the bottom 40% of India’s population, the scheme covers approximately 12.37 crore families—benefiting nearly 55 crore individuals. In a landmark expansion on 29th October 2024, the government introduced Ayushman Vay Vandana, that is extending the AB-PMJAY benefits to all senior citizens aged 70 and above, regardless of their income or socio-economic status. Under the Ayushman Vay Vandana scheme, over 58 lakh senior citizens have enrolled, with more than 2.67 lakh treatments worth ₹496 crore already availed. Requiring only Aadhaar for registration, the scheme ensures easy and accessible healthcare for the 70+ age group. This move recognizes the health vulnerabilities of the elderly and ensures dignified, worry-free treatment in their later years.
Not just this, this scheme also targets the frontline heroes of India’s public health system, ASHA workers, Anganwadi Workers (AWWs), and Anganwadi Helpers (AWHs) ensuring their health and wellbeing as they serve the nation. AB-PMJAY is not just a health scheme—it is a social revolution in healthcare access, empowering India’s most vulnerable with dignity, care, and financial protection.
- Ayushman Bharat Digital Mission (ABDM)
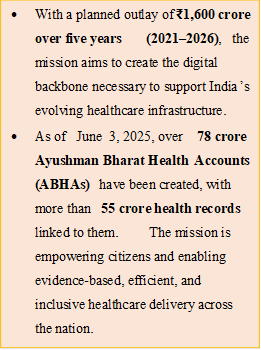
- With a planned outlay of ₹1,600 crore over five years (2021–2026), the mission aims to create the digital backbone necessary to support India’s evolving healthcare infrastructure.
- As of June 3, 2025, over 78 crore Ayushman Bharat Health Accounts (ABHAs) have been created, with more than 55 crore health records linked to them. The mission is empowering citizens and enabling evidence-based, efficient, and inclusive healthcare delivery across the nation.
- With the success of CoWIN and Aarogya Setu, the power of technology in healthcare has been seen.
|
The Government of India launched the Ayushman Bharat Digital Mission (ABDM) to establish a robust and integrated digital health ecosystem across the country. ABDM bridges the gaps between different stakeholders in the healthcare ecosystem—patients, providers, and policymakers—through secure, interoperable digital platforms. At the heart of the mission is the Ayushman Bharat Health Account (ABHA), which allows citizens to digitally link and manage their health records for seamless, paperless access to services.
Recognizing India’s digital diversity, the mission also offers assisted and offline modes for ABHA creation in areas with limited internet connectivity or digital access. Popular applications like the ABHA app and Aarogya Setu have been integrated to further simplify usage and ensure accessibility.
- Pradhan Mantri - Ayushman Bharat Health Infrastructure Mission (PM-ABHIM)
The Pradhan Mantri Ayushman Bharat Health Infrastructure Mission (PM-ABHIM) is a landmark Centrally Sponsored Scheme, with select Central Sector (CS) components, launched with a total outlay of ₹64,180 crore for the period 2021–22 to 2025–26. This transformative initiative aims to strengthen and integrate health service delivery across all levels—primary, secondary, and tertiary care—while building a robust health system capable of effectively responding to current and future pandemics, public health emergencies, and disasters. As part of the Central Sector components, the construction of Critical Care Hospital Blocks (CCHBs) has been sanctioned in 12 central institutions, which are currently at various stages of development. Together, these efforts represent a new generation of health sector reforms focused on delivering a seamless, resilient, and responsive continuum of care across the country.
National Heath Mission (NHM)
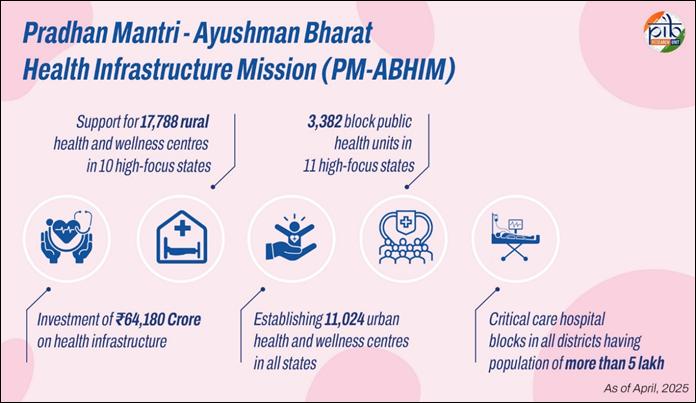
The National Health Mission (NHM), with its two sub-missions — National Rural Health Mission (NRHM) and National Urban Health Mission (NUHM) — is the flagship programme of the Ministry of Health and Family Welfare. It aims to provide universal access to affordable, equitable, and quality healthcare, supporting States/UTs in strengthening public health systems. All NHM services are available free of cost at public health facilities across sub-district and district levels.
The NHM envisages achievement of universal access to equitable, affordable & quality health care services that are accountable and responsive to people’s needs. It serves as the primary vehicle to achieve the goals of NHP 2017 and progress towards Sustainable Development Goal 3 (SDG 3) — “Ensure healthy lives and promote well-being for all at all ages,” including the critical objective of Universal Health Coverage (UHC). The National Health Mission (NHM) encompasses its two Sub-Missions, The National Rural Health Mission (NRHM) and The National Urban Health Mission (NUHM).
In continuation of NHM, the government introduced the National Health Policy (NHP), 2017 which outlines a transformative vision for India’s healthcare system — “the attainment of the highest possible level of health and well-being for all at all ages”. It emphasizes a preventive and promotive approach, embedded in all development strategies, and guarantees universal access to quality healthcare services without financial hardship.
- Budgetary Commitment & Expansion of NHM Services
The Government has significantly scaled up investment and services under NHM over the past decade.
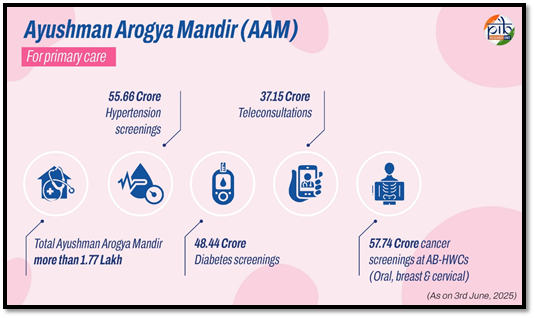
- Transforming Primary Healthcare: Ayushman Arogya Mandirs
A major pillar of universal health coverage is the establishment of Ayushman Arogya Mandirs (AAMs) — formerly known as Ayushman Bharat-Health & Wellness Centres.
- Major Programmes / Schemes under NHM
NHM encompasses a wide range of health programmes to address key health challenges. In the area of Reproductive, Maternal, Neonatal, Child, and Adolescent Health (RMNCH+A), major schemes include Janani Shishu Suraksha Karyakaram (JSSK), Rashtriya Kishor Swasthya Karyakram (RKSK), Rashtriya Bal Swasthya Karyakram (RBSK), the Universal Immunisation Programme, Mission Indradhanush, Janani Suraksha Yojana (JSY), Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA), Navjaat Shishu Suraksha Karyakram (NSSK), the National Programme for Family Planning, and the LaQshya programme for improving quality of care in labour rooms.
To tackle nutritional deficiencies, the mission runs initiatives such as the National Iodine Deficiency Disorders Control Programme, MAA (Mothers’ Absolute Affection) programme for infant and young child feeding, the National Programme for Prevention and Control of Fluorosis (NPPCF), and the National Iron Plus Initiative for anaemia control.
In the realm of communicable diseases, key programmes include the Integrated Disease Surveillance Programme (IDSP), Revised National Tuberculosis Control Programme (RNTCP), National Leprosy Eradication Programme (NLEP), National Vector Borne Disease Control Programme (NVBDCP), National AIDS Control Programme (NACP), Pulse Polio Programme, National Viral Hepatitis Control Program (NVHCP), National Rabies Control Programme, and the National Programme on Containment of Anti-Microbial Resistance (AMR).
To address the growing burden of non-communicable diseases, NHM supports the National Tobacco Control Programme (NTCP), National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS), National Programme for Control and Treatment of Occupational Diseases, National Programme for Prevention and Control of Deafness (NPPCD), National Mental Health Programme, National Programme for Control of Blindness and Visual Impairment (NPCB&VI), Pradhan Mantri National Dialysis Programme (PMNDP), National Programme for Health Care for the Elderly (NPHCE), National Programme for Prevention and Management of Burn Injuries (NPPMBI), and the National Oral Health Programme.
- National TB Elimination Programme (NTEP)
India has made strong progress in eliminating tuberculosis under the National TB Elimination Programme (NTEP). As per the Global TB Report 2024, TB incidence dropped by 17.7% (from 237 to 195 per lakh population) and TB deaths reduced by 21.4% (from 28 to 22 per lakh) between 2015 and 2023. Treatment coverage improved from 53% to 85%, showing major advances in access to care. In 2024, India reported a record 26.17 lakh TB cases, a 69% increase in notifications since 2014. The private sector played a major role, with notifications rising from 1.06 lakh to 9.50 lakh. The treatment success rate also improved from 85% to 89% over the last decade. To support faster diagnosis, Microscopy Centres increased by 88%, and 8,540 molecular labs (NAAT) were set up. A shorter 6-month BPaLM regimen was introduced for drug-resistant TB, improving treatment outcomes. TB Preventive Treatment (TPT) was expanded to all household contacts, with 25 lakh people covered in 2024 using shorter regimens like 3HP and 1HP. The Cy-Tb skin test was launched for early detection in adults.
Under the Nikshay Poshan Yojana, ₹3,607 crore has been provided to 1.23 crore TB patients, with monthly support doubled to ₹1,000 from November 2024. Community support has surged through the Ni-kshay Mitra initiative, with over 2.5 lakh Mitras, 13.23 lakh patients supported, and 29.14 lakh food baskets distributed. A major drive, the 100-Day TB Mukt Bharat Abhiyan (Dec 2024–Mar 2025), covered 347 districts, mobilized 30,000+ leaders, and screened 12.97 crore people through 13.46 lakh health camps, identifying 7.19 lakh TB cases, including 2.85 lakh asymptomatic ones.
- National Sickle Cell Anaemia Elimination Mission
National Sickle Cell Anaemia Elimination Mission was launched by Prime Minister Shri Narendra Modi in July 2023. The Mission sets an ambitious target to eradicate sickle cell disease by 2047, focusing on awareness generation, universal screening, and comprehensive disease management among tribal populations through a community-centric and integrated approach. As of 3rd June, 2025, a total of 5.72 crore people have been screened for Sickle Cell Disease, achieving over 75% of the three-year target. Notably, more than 2.65 crore screenings were conducted in just one year since April 2024. States have issued 2.50 crore sickle cell status cards, helping to identify 1.98 lakh diseased patients and 14 lakh individuals with the sickle cell trait. All diagnosed patients are currently receiving appropriate treatment.
- Pradhan Mantri National Dialysis Programme (PMNDP)
PMNDP has been implemented in total 36 States/UT in 749 (48 linked) Districts at 1674 centres by deploying 11757 hemo-dialysis machines. A total of 27.86 lakh patient (cumulative) availed dialysis services and 342.25 Lakh Hemo-dialysis sessions (cumulative) held as on 03.06.2025. Pradhan Mantri National Dialysis Program (PMNDP) has, so far resulted in Total Out of Pocket Expenditure savings of Rs. 8000 Crore and an additional savings of Rs. 8000 Crore under dialysis through PMJAY.
- National Free Drugs Service Initiative and National Free Diagnostic Service Initiative
The initiative ensures the availability of essential drugs and diagnostic facilities to reduce out-of-pocket expenditure.
- Comprehensive Cancer Care
In response to the rising burden of cancer in India, the Government has adopted a robust multi-tiered strategy—focusing on early detection, infrastructure development, and affordable treatment, in line with the goals of Universal Health Coverage.
Early diagnosis remains the cornerstone of cancer control. Under the National Health Mission (NHM), large-scale screening programs at the primary healthcare level have led to significant improvements in early cancer detection based on National NCD Portal as on 1st June, 2025:
- Oral Cancer: Over 31.70 crore screenings
- Breast Cancer: Over 16.68 crore screenings
- Cervical Cancer: Over 9.97 crore screenings
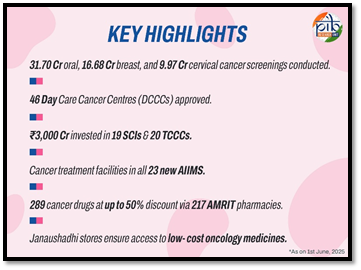
These screenings are primarily carried out at Ayushman Arogya Mandirs (Health and Wellness Centres), bringing preventive care to the community’s doorstep. To enhance access to treatment, a strong secondary and tertiary care infrastructure is being developed. Following a Budget announcement, a gap analysis based on district-level cancer burden was carried out, leading to the approval of 46 Day Care Cancer Centres (DCCCs) under NHM’s Programme Implementation Plan (PIP). These centres are being established in district hospitals to decentralize care and reduce patient load on tertiary facilities.
At the tertiary level, the Government has invested over ₹3,000 crore in the past decade for the development of 19 State Cancer Institutes and 20 Tertiary Cancer Care Centres. Cancer treatment facilities have also been established in all 23 new AIIMS, while premier institutions like the National Cancer Institute (NCI) in Jhajjar and the Second Campus of Chittaranjan National Cancer Institute (CNCI) have been set up to further strengthen the national cancer care ecosystem. Ensuring affordability has been a key pillar of this strategy. Through 217 AMRIT pharmacies, 289 cancer medicines are made available at discounts of up to 50%. Additionally, the Pradhan Mantri Bhartiya Janaushadhi Pariyojana plays a vital role in providing affordable anti-cancer drugs to the public.
Making Health Services Reach All
- Making Medicines Affordable
Ensuring access to affordable medicines for all has been a central pillar of India’s healthcare reforms over the past decade. Recognizing that high medical costs, particularly for essential drugs, often push families into financial hardship, the Government of India has implemented targeted initiatives to make quality medicines available at significantly reduced prices—transforming the healthcare experience for millions of citizens.
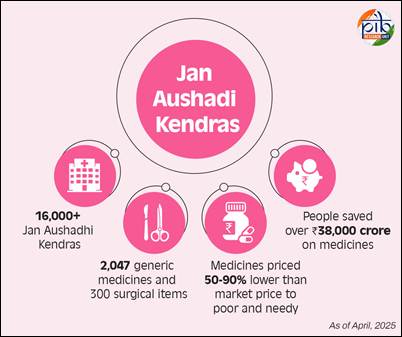
A key intervention in this regard is the Pradhan Mantri Bhartiya Janaushadhi Pariyojana (PMBJP), launched in November 2016 by the Department of Pharmaceuticals. The initiative aims to provide high-quality generic medicines at significantly lower prices through a dedicated network of Jan Aushadhi Kendras. These outlets offer medicines that are equivalent in efficacy and safety to their branded counterparts but cost substantially less—between 50% to 90% lower than market rates. By offering affordable and reliable medications, PMBJP has empowered countless families to seek timely treatment and lead healthier lives.
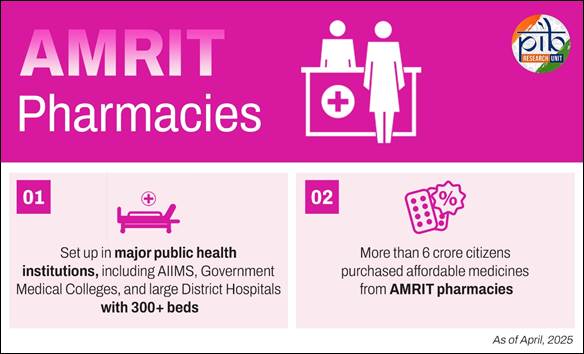
To complement the PMBJP, the government launched the Affordable Medicines and Reliable Implants for Treatment (AMRIT) initiative, aimed specifically at supporting tertiary healthcare. AMRIT Pharmacies act as centralized supply points for branded, branded-generic, and generic drugs, as well as surgical items, consumables, and medical implants—especially those required for high-end treatments.
- Bridging the Digital Health Divide
- eSanjeevani- National Telemedicine Service
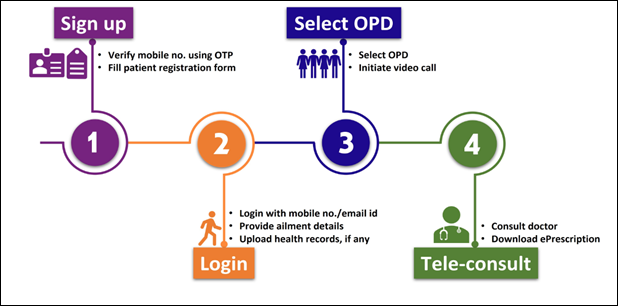
The government’s telemedicine programme – eSanjeevani is bringing a revolution in the health sector of the country. eSanjeevani facilitates quick and easy access to doctors and medical specialists from your
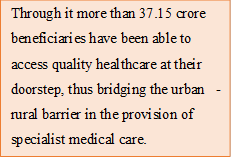
Through it more than 37.15 crore beneficiaries have been able to access quality healthcare at their doorstep, thus bridging the urban-rural barrier in the provision of specialist medical care.
|
smartphones. You can also access quality health services remotely via eSanjeevani by visiting the nearest Ayushman Bharat Health & Wellness Centre.
Child and Maternal Health
- Universal Immunization Programme (UIP)
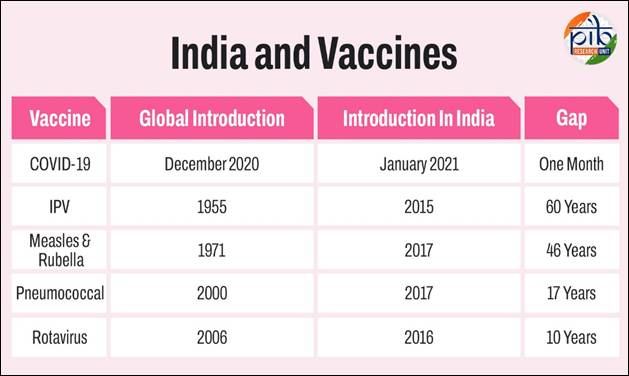
India has made remarkable strides in advancing maternal and child health through a series of comprehensive public health programmes, digital innovations, and legal reforms. At the heart of these efforts lies the Universal Immunization Programme (UIP), one of the world’s largest and most ambitious public health initiatives.
Every year, UIP targets 2.6 crore newborns and 2.9 crore pregnant women, aiming to ensure that every child is fully immunized in their first year of life.
A child is considered fully immunized when they receive all vaccines scheduled under the National Immunization Schedule—including BCG, three doses of Oral Polio Vaccine (OPV), three doses of Pentavalent vaccine, and the first dose of the Measles-Rubella (MR) vaccine.
As a result of sustained efforts and outreach, India’s Full Immunization Coverage (FIC) has reached an impressive 94.1%, reflecting the government’s strong commitment to preventive healthcare.
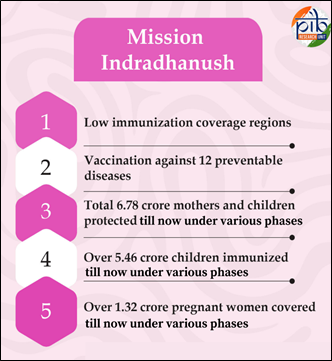
A pivotal initiative in this regard is Mission Indradhanush which was launched on 25th December 2014 as a special catch-up vaccination campaign under the Universal Immunization Programme (UIP). Mission Indradhanush specifically targets children and pregnant women who have either missed or dropped out of routine immunization schedules, focusing on regions with low vaccination coverage. Through multiple phases, the campaign ensures that no child is left behind in receiving life-saving vaccines.
To further enhance efficiency and accountability in immunization delivery, the government launched the U-WIN platform, a digital initiative under UIP.
As of 30th May 2025, 10.48 crore beneficiaries have been registered on U-WIN, with 93.91 lakh deliveries, 1.88 crore vaccination sessions, and a total of 41.73 crore vaccine doses recorded.
This platform has become a critical tool in ensuring transparency, improving service delivery, and reaching underserved populations.
Complementing the UIP are three flagship maternal health schemes that focus on encouraging institutional deliveries and providing respectful, dignified care. Under the Janani Shishu Suraksha Karyakaram (JSSK), launched to promote free institutional delivery and neonatal care, more than 16.60 crore beneficiaries have been served since 2014–15. Simultaneously, the Janani Suraksha Yojana (JSY), which incentivizes institutional deliveries through conditional cash transfers, has benefitted over 11.07 crore women as of March 2025. Adding to this, the Surakshit Matritva Aashwasan (SUMAN) initiative has strengthened respectful and quality care for pregnant women, with 90,015 SUMAN health facilities notified across India by March 2025.
The Medical Termination of Pregnancy (Amendment) Act, 2021 is a landmark reform that empowers women with the right to make informed reproductive choices. It expands access to safe and legal abortion services, ensuring women from all backgrounds can seek care in a regulated, rights-based healthcare system.
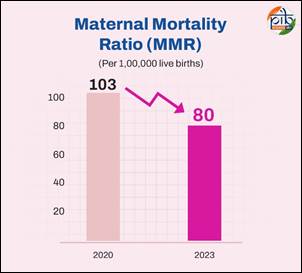
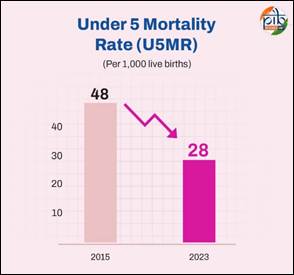
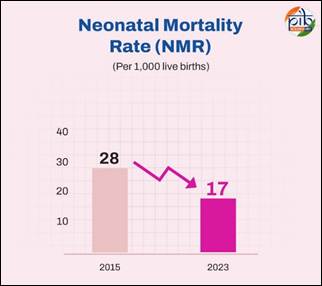
These efforts have yielded powerful health outcomes. According to the United Nations Maternal Mortality Estimation Inter-Agency Group (UN-MMEIG) Report for 2000–2023, India’s Maternal Mortality Ratio (MMR) dropped from 103 per lakh live births in 2020 to 80 per lakh live births in 2023, marking a significant 23-point reduction in just three years. Similarly, the UN Inter-Agency Group for Child Mortality Estimation (UN IGME) reported in March 2025 that under-five mortality in India fell from 48 to 28 per 1,000 live births between 2015 and 2023—a 42% decline, which far outpaces the global average of 14%. Neonatal mortality during the same period decreased from 28 to 17 per 1,000 live births, a 39% reduction, compared to a global average of 11%.
These statistics reflect India’s steadfast progress in improving child survival, earning global recognition, with UN IGME identifying India as an exemplar in reducing child mortality through effective strategies and policies.
Medical education and Public health
Over the past 11 years, the Modi government has brought transformative change to India's medical education and public health landscape, addressing deep-rooted challenges and making quality healthcare education more accessible. Earlier, aspiring medical students—especially those from rural and modest backgrounds—faced formidable barriers, including a lack of government medical colleges, unaffordable private institution fees, and opaque, corruption-ridden admission processes.
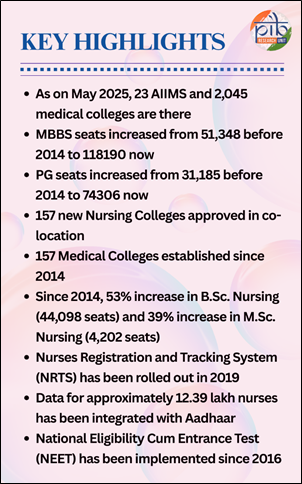
To rectify this, the government launched bold and systemic reforms. A cornerstone of this effort was the establishment and expansion of AIIMS across multiple states, including the first-ever AIIMS in the Northeast (Assam). As on May 2025, there are 23 AIIMS and 2,045 medical colleges in India including includes 780 Allopathy, 323 Dental, and 942 AYUSH institutions. MBBS seats increased by 130% (from 51,348 to 1,18,190), while PG seats grew by 138% (from 31,185 to 74,306)—ensuring a larger, continuous supply of trained doctors.
To further strengthen the health workforce, the government approved 157 co-located nursing colleges, alongside the new medical colleges. As of April 2025, funding has been released for 106 such nursing institutions. Simultaneously, B.Sc. Nursing seats rose by 53% to 1,27,290 and M.Sc. Nursing seats increased by 39% to 14,986, enhancing both reach and depth of nursing education. In 2019, the Nurses Registration and Tracking System (NRTS) was launched, bringing over 12.39 lakh nurses into a digitally verified, Aadhaar-linked national database—streamlining regulation and workforce management.
In a historic move to clean up medical education and promote merit, the Medical Council of India was replaced by the National Medical Commission (NMC) through the National Medical Commission Act, 2019. Several other landmark legislations were enacted to modernize health education:
- National Commission for Allied and Healthcare Professions Act, 2021
- National Dental Commission Act, 2023
- National Nursing and Midwifery Commission Act, 2023
The introduction of NEET in 2016 ensured a uniform and transparent admission process, establishing meritocracy across medical institutions.
In line with evolving healthcare demands, competency-based curricula for 10 allied health professions have been rolled out under the NCAHP, standardizing learning outcomes and enhancing care delivery. To encourage research and academic excellence in the nursing domain, the National Consortium for Ph.D. in Nursing was constituted by the Indian Nursing Council in October 2024, marking a new chapter in evidence-based nursing practice and innovation.
India’s Response During COVID-19
India’s response to the COVID-19 pandemic has emerged as one of the most proactive, comprehensive, and people-first strategies in the world. Guided by foresight and swift action, the country launched a nationwide mobilisation to protect lives, contain the virus, and build long-term healthcare resilience.
- Proactive Leadership and Early Interventions
Long before the global alarm bells rang, India had already taken critical preventive steps. Airport screenings began even before the first domestic case was reported, underscoring the government’s alertness. In a significant display of responsible leadership, Prime Minister Narendra Modi refrained from attending Holi celebrations as early as the first week of March 2020, urging the nation to avoid large gatherings.
Mask mandates were enforced across several states well before the World Health Organization (WHO) issued any global advisories. India was also among the first nations to introduce Rapid Antigen Tests, expediting diagnosis and containment ahead of WHO guidelines.
While the world was still grappling with rising death tolls, India had already formed a dedicated COVID-19 vaccine task force in April 2020, laying the groundwork for what would become the world's most extensive vaccination campaign. The early and strategically timed nationwide lockdown bought the country valuable time to ramp up medical infrastructure and prepare for the battle ahead—a decision widely acknowledged by global experts.
- The World’s Largest Vaccination Drive
India’s COVID-19 vaccination campaign stands as a monumental public health achievement. Powered by indigenously developed vaccines and supported by a robust digital infrastructure like CoWIN, India successfully administered over 2.2 billion doses of Covid vaccine doses, a feat unmatched globally in terms of scale and speed. It marked a turning point in India’s healthcare journey, showcasing the nation’s capability to deliver last-mile healthcare in real-time. India’s National Covid-19 Vaccination Programme, which is the world’s largest vaccination programme, began on 16 January 2021, initially with the aim of covering the adult population of the country in the shortest possible time. The programme was expanded to include all persons aged 12 years and above and for the precautionary dose for all persons aged 18 years and above.
- Historic Infrastructure Ramp-Up
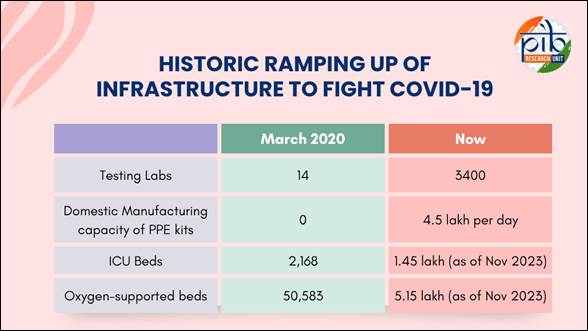
India’s pandemic response was not limited to medical treatment—it was equally defined by massive infrastructure expansion and innovative solutions:
- Oxygen Express Trains: Indian Railways operated nearly 900 Oxygen Express trains, transporting over 36,840 tonnes of liquid medical oxygen to severely affected states. This swift action was instrumental during the peak of the second wave.
- Indian Air Force Deployment: The Indian Air Force was mobilized to airlift cryogenic oxygen tankers and essential medical equipment, cutting down crucial transport time and ensuring timely support.
- Isolation Coaches: In a creative use of existing assets, 4,176 railway coaches were converted into fully functional isolation and quarantine facilities, significantly enhancing patient capacity across the country.
- Makeshift Quarantine Facilities: Paramilitary forces and central agencies established and operated temporary quarantine centres in both urban and remote regions, enabling quicker isolation and recovery.
- PSA Oxygen Plants: The government sanctioned over 1,563 Pressure Swing Adsorption (PSA) oxygen plants, enhancing oxygen availability and making healthcare facilities more self-sufficient, especially in rural and underserved areas.
- Emergency COVID Response Package (ECRP)
To further reinforce the healthcare ecosystem, the Government of India launched the Emergency COVID Response Package (ECRP) in two phases:
- Under ECRP-I, a total of ₹8,584.33 crore was released.
- Under ECRP-II, another ₹12,740.22 crore was allocated.
These funds, disbursed through the National Health Mission (NHM), were used to upgrade existing healthcare infrastructure, add ICU beds, procure ventilators, enhance laboratory networks, and expand testing and surveillance capacity.
Conclusion
India’s healthcare transformation over the past 11 years has been both comprehensive and compassionate. Guided by the vision of “Health for All,” the government has made unprecedented strides in expanding access, improving quality, and ensuring affordability. Landmark initiatives like Ayushman Bharat, PM-ABHIM, and eSanjeevani have brought medical care closer to the people—especially in rural and underserved regions. Investments in infrastructure, digital health, immunization, maternal and child care, and medical education have created a robust foundation for future health security. This progress is not just about numbers—it is about lives improved, dignity restored, and hope renewed. As India steps into Amrit Kaal, the focus remains firm on inclusive, resilient, and people-centric healthcare. The message is clear: every life matters, and a healthier India is a stronger India.
References:
Click here for pdf file
***
Explainer 16/ Series on 11 Years of Government
Santosh Kumar/ Sarla Meena/ Priya Nagar
(Explainer ID: 154668)
आगंतुक पटल : 12909
Provide suggestions / comments